Tarrytown (NY)- July 01, 2005 – OmniMD™ (www.omnimd.com) of Tarrytown, New York announces an important advance in solving one of the most time-consuming and costly administrative burdens faced by most medical offices: Verifying patients' eligibility for insurance.
The Problem:
Three out of every four insurance denials are due to problems with eligibility verification: According the AMA Council on Medical Service, almost half of physicians surveyed reported that more than 10 percent of insurance claims are denied retrospectively and many more are down-coded. On top of this, medical practice staff spend far too much time resolving insurance issues and on bill collection. Patient eligibility verification presents a huge administrative burden on medical offices requiring numerous telephone calls to and from insurance companies leaving stacks of unprocessed claims. The Solution:
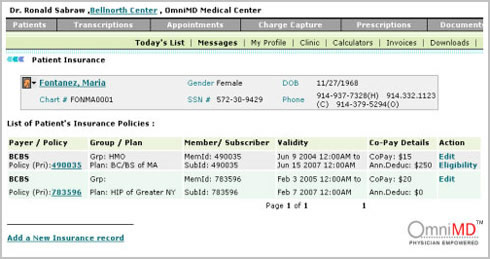
OmniMD™, a leading provider of HIPAA-compliant Electronic Medical Record (EMR) programs and services has released its newest program for verifying patient's insurance data over the Internet to make the process more efficient while decreasing the rate of insurance denials and write-offs. In fact, many providers are now offering access to their database of enrollees through the internet to help the medical office verify that a patient is actually covered.
OmniMD™ online insurance eligibility checking service enables the medical office to check a patient's current eligibility for healthcare benefits before he or she arrives at the point-of-care by linking the eligibility check with the appointment scheduler.
The system eliminates the need for paper transactions while providing an accurate determination of the patient's co-pay and deductibles, clarifying the patient's coverage expectations and reducing the risk of uncollected balances. |